Global Journal of Medical and Clinical Case Reports
Spiked Helmet Sign in a Patient with Septic Shock after Ivor-Lewis Esophagectomy
1Cardiology Service, University Hospital of Toledo, USA
2Anesthesiology and Resuscitation Service, University Hospital of Toledo, USA
Author and article information
Cite this as
Pelegrini NN, Domingo JC, Garcia-Cano Escondrillas B, Gil JZ, Avila Sánchez FJ, Arias Palomares MÁ, et al. Spiked Helmet Sign in a Patient with Septic Shock after Ivor-Lewis Esophagectomy. Glob J Medical Clin Case Rep. 2025:12(9):194-196. Available from: 10.17352/gjmccr.000225
Copyright License
© 2025 Pelegrini NN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Case summary
A 49-year-old former smoker with no significant medical history presented with several months of oral intolerance, nausea, and a 20-kg weight loss. An upper endoscopy revealed a mid-to-distal esophageal adenocarcinoma, confirmed by biopsy. Staging showed no metastasis, and the patient underwent neoadjuvant FLOT chemotherapy followed by Ivor-Lewis esophagectomy.
Initially, the postoperative course was stable, but on POD 6, the patient developed pleuritic chest pain, mild hypotension, and oxygen desaturation. Imaging identified a proximal esophagogastric anastomotic leak. Urgent surgery confirmed a 4–5 mm necrotic defect with right-sided subpleural leakage. A negative-pressure esophageal sponge and a chest drain were inserted due to an intraoperative right pneumothorax. The patient was transferred to the ICU, intubated on volume-controlled mechanical ventilation, and required norepinephrine for hemodynamic support. Empirical antibiotic and antifungal therapy (meropenem, linezolid, and anidulafungin) was initiated due to septic parameters (CRP 294 mg/L; PCT 6.37 ng/mL). Subsequently, purulent drainage was observed in the right chest tube, with cultures isolating Streptococcus anginosus and Stenotrophomonas maltophilia. The patient developed worsening septic shock, requiring increased vasopressor support and recruitment maneuvers. A tracheostomy was performed due to expected prolonged mechanical ventilation.
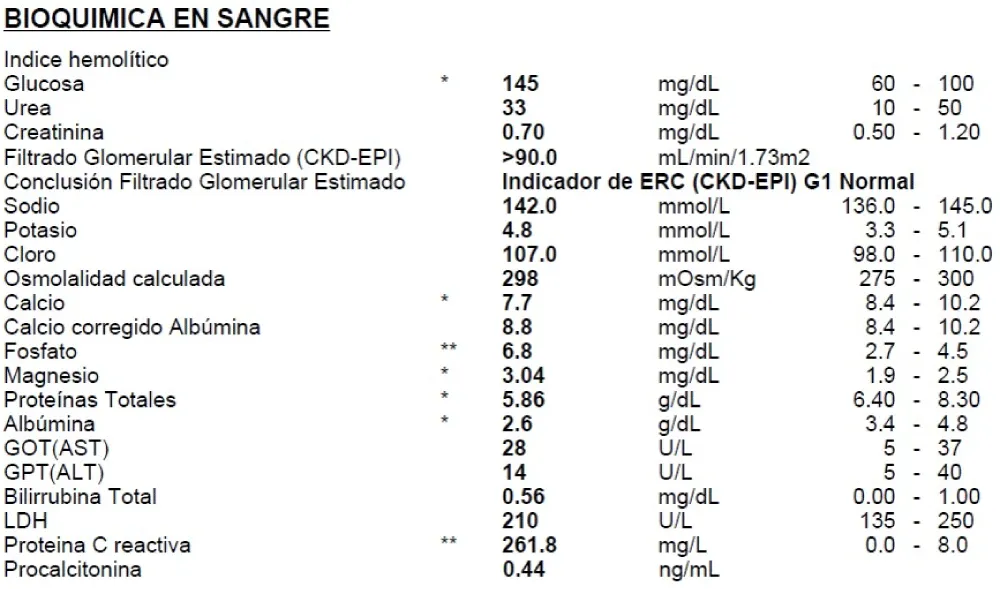
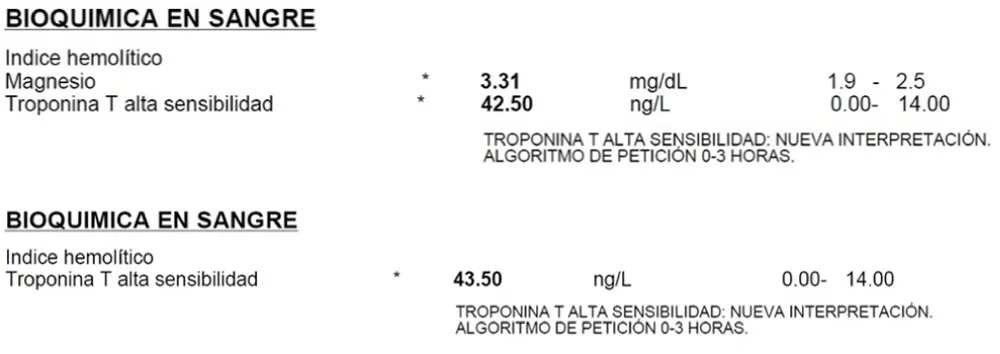
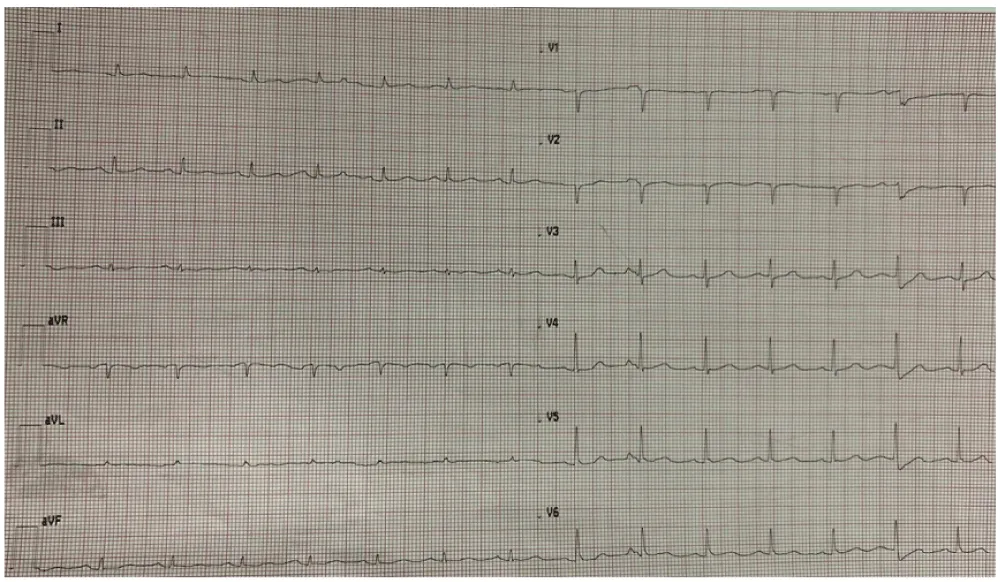
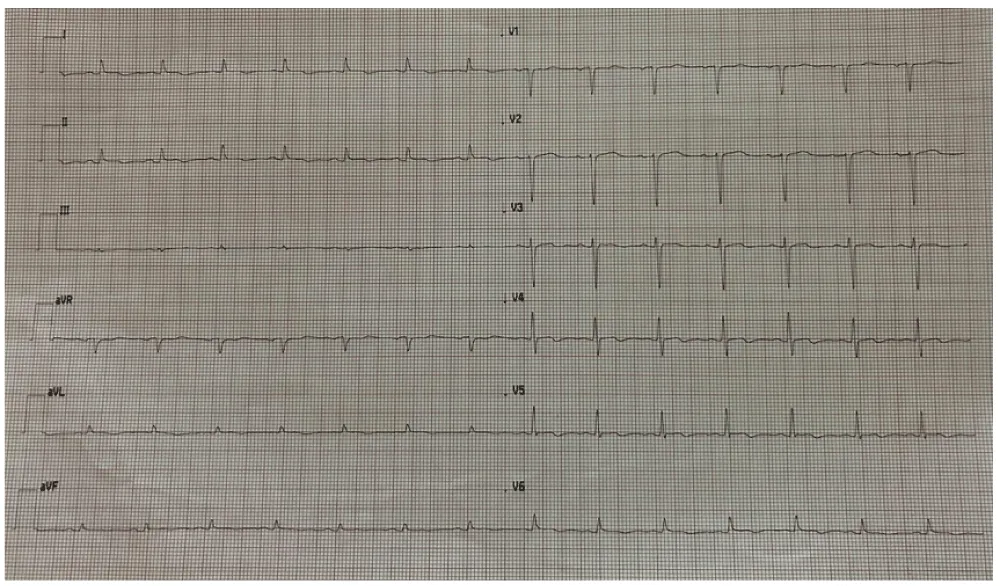
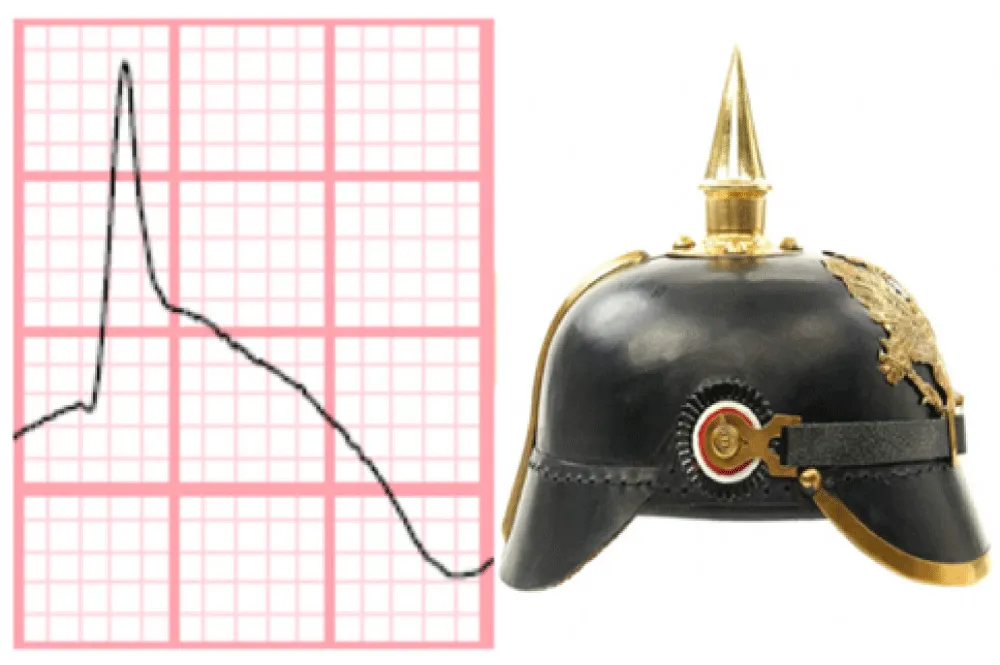
On ICU day 7, the ECG monitor showed significant QRS morphology changes. A 12-lead ECG (Image 4) revealed sinus rhythm at 85 bpm, PR interval 200 ms, normal axis, QRS 110 ms, ST-segment elevation in leads I, aVL, II, III, aVF, V5–V6, ST depression in V1–V4, and negative T waves in I, aVL, V5–V6. QTc was prolonged to 520 ms. Bedside echocardiography showed preserved biventricular function (LVEF 60%), no regional wall motion abnormalities were observed, no significant valvular disease, and a small, subacute pericardial effusion without signs of tamponade. Serial high-sensitivity troponin I levels were 42.5 ng/L and 43.5 ng/L three hours apart (Image 2). No dynamic changes were observed. Laboratory tests revealed metabolic acidosis (pH 7.21, HCO3 17.2 mmol/L), mild hypermagnesemia (3.31 mg/dL), and hyperphosphatemia (4.7 mg/dL). Sodium, chloride, and calcium levels were within the normal range (142 mmol/L, 107 mmol/L, and 8.8 mg/dL, respectively, as shown in Image 1). Notably, metoclopramide and erythromycin had been initiated that same day. Inflammatory markers remained markedly elevated (Images 1-5).
Differential diagnosis
Given the absence of structural heart disease, stable troponin levels, and lack of echocardiographic findings suggestive of myocardial infarction, the ECG abnormalities were attributed to the Spiked Helmet Sign (SHS). In this particular case, a distinctive feature was the presence of an inverted helmet-like morphology in leads V1, V2, and V3, which is a less commonly described presentation of SHS. This rare ECG pattern is not indicative of primary cardiac pathology but rather serves as a marker of critical systemic illness [1]. It is thought to result from excessive sympathetic activity increasing ventricular repolarization dispersion, leading to QT prolongation and ST-T segment changes [1]. In this case, SHS likely developed in the context of septic shock following anastomotic dehiscence, with contributing factors including increased intrathoracic pressure from pneumothorax, empyema, and prolonged mechanical ventilation, as well as electrolyte imbalances and QT-prolonging Medications.
Clinical course
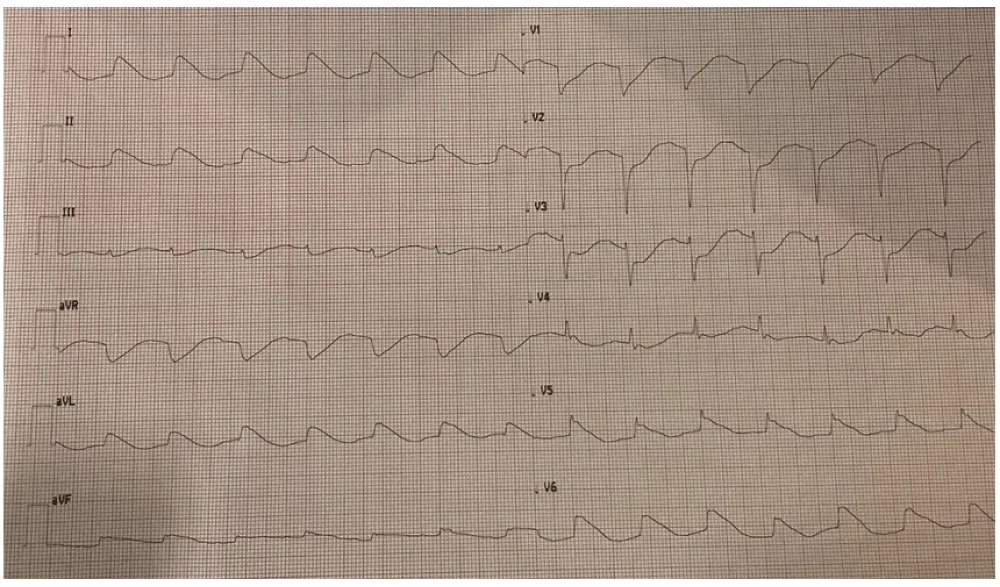
Within 24 hours, as the patient’s hemodynamics stabilized and inflammatory markers decreased, serial ECGs (Image 5) showed progressive normalization of repolarization changes, ultimately returning to baseline with sinus rhythm, a narrow QRS, and residual signs of chamber overload. A metallic esophageal stent was subsequently placed. Unfortunately, the patient later developed acute respiratory distress syndrome requiring prone positioning, though no new ECG changes were observed. At the time of writing, the patient remains hospitalized.
Discussion
The Spiked Helmet Sign (SHS), also known as the “Pickelhaube sign,” derives its name from its resemblance to the pointed Prussian military helmet, with dome-and-spike ST-segment elevation preceding the QRS [1]. First reported in 2011 by Littmann, et al. [2], it has been increasingly associated with non-cardiac, life-threatening conditions [2]. A 2023 systematic review included 39 patients, with 19 deaths. Subsequent reports brought the total to 52 cases, with male patients exhibiting higher mortality [3-14]. Although the precise pathophysiology remains unclear, proposed mechanisms include abnormal diaphragmatic contractions due to acute intrathoracic or intra-abdominal pressure changes, vagal stimulation, and sympathetic overdrive [1,14]. SHS has been observed in intracranial hemorrhage, pulmonary disease, gastric distention, abdominal pathology, and, as in our case, postsurgical septic shock [1]. Prompt recognition is essential, as SHS may signal severe underlying disease even in the absence of cardiac involvement.
To our knowledge, this is one of the very few documented cases of SHS associated with anastomotic leakage following esophagectomy, highlighting the relevance of electrocardiographic vigilance in critically ill patients ((Image 6).
References
- Wang G, Zhong S, Chu H, Zhong L. Spiked Helmet Sign: An Uncommon Electrocardiographic Marker. Rev Cardiovasc Med. 2023;24(9):272. Available from: https://doi.org/10.31083/j.rcm2409272
- Littmann L, Monroe MH. The "spiked helmet" sign: a new electrocardiographic marker of critical illness and high risk of death. Mayo Clin Proc. 2011;86:1245-1246. Available from: https://doi.org/10.4065/mcp.2011.0647
- Mahmoudi E, Hui JMH, Leung KSK, Satti DI, Lee YHA, Li KHC, et al. Spiked helmet electrocardiographic sign—a systematic review of case reports. Curr Probl Cardiol. 2023;48:101535. Available from: https://doi.org/10.1016/j.cpcardiol.2022.101535
- Markson F, Shalak M, Kesiena O, Shamaki GR, Ekanem E, Ong K. "The Spiked Helmet sign": A harbinger of impending barotrauma. Heart Lung. 2023;57:203-206. Available from: https://doi.org/10.1016/j.hrtlng.2022.09.022
- Al Saiegh Y, Liskov S, Yan GX. Spiked Helmet Sign in the Inferior Leads. JAMA Intern Med. 2023;183(9):1007-1008. Available from: https://doi.org/10.1001/jamainternmed.2023.1728
- Narvaez-Guerra O, Osorio B, Gentile B, Del-Carpio Munoz F. Electrocardiographic spiked-helmet sign in critical non-cardiac illness. BMJ Case Rep. 2023;16(10):e254546. Available from: https://doi.org/10.1136/bcr-2022-254546
- Sasmita BR, Luo S, Huang B. Electrocardiographic semi-spiked helmet sign in critically Ill patients: A case series. Medicine (Baltimore). 2023;102(43):e35661. Available from: https://doi.org/10.1097/md.0000000000035661
- Fall S, Farhat SB, Chelly A, Kaddour H, Saad SB, El Hedi AM, et al. The spiked helmet sign in a patient with erysipelas: an alarming electrocardiogram sign (a case report). Pan Afr Med J. 2023;46:58. Available from: https://doi.org/10.11604/pamj.2023.46.58.40438
- Yan BW, Yip D, Mallidi J, Goldschlager N. Dynamic "spiked helmet sign": Further evidence for prolonged QT. J Electrocardiol. 2024;84:91-94. Available from: https://doi.org/10.1016/j.jelectrocard.2024.03.014
- Kang Moreira E, Loor Sabando C, Gilbert Orús MD, Morejón Barragán P, Barrera Rivera M, et al. Sympathetic fire and rhythm of death "Spiked Helmet" in the Takotsubo cardiomyopathy. Case report. Arch Peru Cardiol Cir Cardiovasc. 2024;5(3):176-180. Available from: https://doi.org/10.47487/apcyccv.v5i3.367
- Hwang E, Namburar S, Siegel M, Sanchez A. Takotsubo cardiomyopathy and cardiogenic shock due to hypokalaemic rhabdomyolysis. BMJ Case Rep. 2024;17(10):e261456. Available from: https://doi.org/10.1136/bcr-2024-261456
- Dai C, Chen ZE, Wu SL, Xue YM, Liu FZ. Diaphragmatic hernia with a nonischemic electrocardiographic presentation of the spiked helmet sign. Heart Rhythm. 2025 May 22:S1547-5271(25)02462-2. Available from: https://doi.org/10.1016/j.hrthm.2025.05.033
- Bosnjak M, Nottingham T, Strey G. A Distinctive Electrocardiographic Pattern: Unveiling the Spiked Helmet Sign. JACC Case Rep. 2025;30(12):103412. Available from: https://doi.org/10.1016/j.jaccas.2025.103412
- Adithiyaa NV, Yeriswamy MC. Spiked-helmet Sign: A Rare but Alarming Sign on Electrocardiogram. J Indian Coll Cardiol. 2024;14(2):71-72. Available from: https://journals.lww.com/jicc/fulltext/2024/14020/spiked_helmet_sign__a_rare_but_alarming_sign_on.6.aspx
- Crinion D, Abdollah H, Baranchuk A. An Ominous ECG Sign in Critical Care. Circulation. 2020;141(25):2106-2109. Available from: https://doi.org/10.1161/circulationaha.120.047427

 Save to Mendeley
Save to Mendeley

