Global Journal of Medical and Clinical Case Reports
Treatment of Nodular Non-Pigmented Basal Cell Carcinoma on the Nose by the Chemical Procedure of Dr. G. Dunkic: A Case Report
1Health Care Clinic Apiderm Plus, Stojana Aralice 6, Belgrade, Serbia
2Institute for Technology of Nuclear and Other Raw Materials, Franše d’ Eperea Boulevard 86, Belgrade, Serbia
3Health Care Clinic Dunkic, Lepenicki Boulevard 1, Kragujevac, Serbia
Author and article information
Cite this as
Djordjevic N, Dunkic A, Djordjevic M. Treatment of Nodular Non-Pigmented Basal Cell Carcinoma on the Nose by the Chemical Procedure of Dr. G. Dunkic: A Case Report. Glob J Medical Clin Case Rep. 2026:13(1):012-015. Available from: 10.17352/gjmccr.000237
Copyright License
© 2026 Djordjevic N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Abstract
Background: Basal Cell Carcinoma (BCC) is the most common malignant skin tumor, frequently affecting sun-exposed areas such as the nose. Surgical excision remains the gold standard, but alternative approaches may be considered in elderly patients or those unwilling to undergo invasive procedures.
Case presentation: We describe an 82-year-old male with a nodular, non-pigmented lesion on the nose, measuring 25 × 15 × 10 mm, present for two years and showing accelerated growth after repeated trauma. Clinical examination confirmed nodular BCC with surface capillaries. The patient refused surgical excision and was treated using a proprietary chemical method developed by Dr. G. Dunkic, et al. A liquid preparation was applied topically without anesthesia or tissue penetration. Within 24–72 hours, a crust formed and detached after 15–20 days, resulting in complete epithelialization. Healing was uneventful, with no major complications.
Conclusion: This case demonstrates the potential of a chemical, non-invasive approach for nodular BCC removal. Further controlled studies are needed to validate efficacy and safety compared to conventional therapies.
Credit: Health Care Clinic Apiderm Plus, Health Care Clinic Dunkic
Restrictions: Not to be used for advertising or in a defamatory context.
The chemical method for removing lesions by Dr. G. Dunkic is proprietary, and unauthorized use is strictly prohibited. The proprietary chemical preparation used in this case is not disclosed in detail due to intellectual property protection. The focus of this report is on the clinical outcome rather than the composition of the agent.
Note on Method Availability: The mole removal method presented in this paper is the result of years of family-based experience and development. Due to its specificity, effectiveness, and practical value, the method is not publicly available for unrestricted use without prior agreement with the authors.
The authors are open to professional collaboration, including licensing, supervised clinical application, and research projects conducted under controlled conditions. Interested parties are invited to contact the authors directly using the information provided in this paper to discuss potential partnerships.
Our goal is to contribute to the advancement of alternative approaches in dermatological practice while preserving the integrity and ownership of the method.
Introduction
Basal cell carcinoma (BCC) is the most common malignant skin tumor, accounting for approximately 80% of non-melanoma skin cancers. It typically arises in sun-exposed areas, particularly the face, and is most prevalent among elderly patients with a history of chronic ultraviolet radiation exposure. The gold standard of treatment is surgical excision, which provides high cure rates and allows histopathological confirmation. Alternative modalities include the chemical method developed by Dr. G. Dunkic [1-3], emollients [4], topical keratolytic treatment [5], chemical peelings [6], photodynamic therapy [7], cryosurgery [8], radiotherapy, electrocautery, etc. However, these approaches may be limited by patient comorbidities, cosmetic concerns, or refusal to undergo invasive procedures.
In this context, we present a case of nodular, non-pigmented BCC of the nose treated with a proprietary chemical method developed by Dr. G. Dunkic. This non-invasive approach, based on topical application of a liquid preparation, has been used for decades in clinical practice and offers a potential alternative for patients unwilling or unable to undergo surgery. This report aims to describe the clinical outcome of this treatment and to discuss its possible role within the spectrum of dermatological therapies.
The global incidence of basal cell carcinoma continues to rise, with more than two million new cases diagnosed annually. This increase is largely attributed to aging populations and cumulative ultraviolet exposure. Lesions located on the nose are particularly challenging due to the cosmetic and functional importance of this area, often requiring careful consideration of both therapeutic efficacy and aesthetic outcomes. Consequently, there is growing interest in exploring less invasive treatment modalities that may provide satisfactory results while minimizing patient discomfort and preserving tissue integrity.
Case presentation
An 82-year-old male patient presented with a nodular, non-pigmented lesion on the nose, measuring 25 × 15 × 10 mm. According to his recollection, the lesion had been present for approximately two years and showed accelerated growth after repeated attempts to remove it mechanically with his fingernail.
Clinical examination revealed a nodular Basal Cell Carcinoma (BCC) with prominent surface capillaries. The patient was advised to undergo surgical excision, which is the standard of care, but he refused due to personal concerns. Consequently, he was referred to Health Care Clinic Dunkic, where a proprietary chemical method developed by Dr. G. Dunkic was applied.
The procedure involved the topical application of a liquid preparation directly onto the lesion surface, without anesthesia or tissue penetration. The patient reported only mild burning sensations during treatment, which did not exceed the pain threshold. Within 24–72 hours, a crust formed at the treated site. The crust detached spontaneously after 15–20 days, accompanied by complete epithelialization.
No major complications were observed, except for occasional secondary local infection in similar cases, which can be managed with topical antibiotics. In this patient, healing was uneventful, and follow-up examination confirmed complete removal of the lesion with minimal scarring.
Discussion
Basal Cell Carcinoma (BCC) is generally managed by surgical excision, which remains the gold standard due to its high cure rates and ability to provide histopathological confirmation. Other established modalities include cryotherapy, radiotherapy, photodynamic therapy, electrocautery, and topical keratolytics. Each of these approaches has specific advantages and limitations, often related to recurrence rates, cosmetic outcomes, and patient tolerance [9-19].
In the present case, the patient refused surgical excision, highlighting the need for alternative, less invasive options. The proprietary chemical method developed by Dr. G. Dunkic represents a non-invasive approach based on the topical application of a liquid preparation. Unlike surgical or ablative techniques, this method does not require anesthesia, does not involve tissue penetration, and is associated with minimal bleeding and scarring. The clinical outcome in this case was favorable, with complete removal of the lesion and satisfactory cosmetic results.
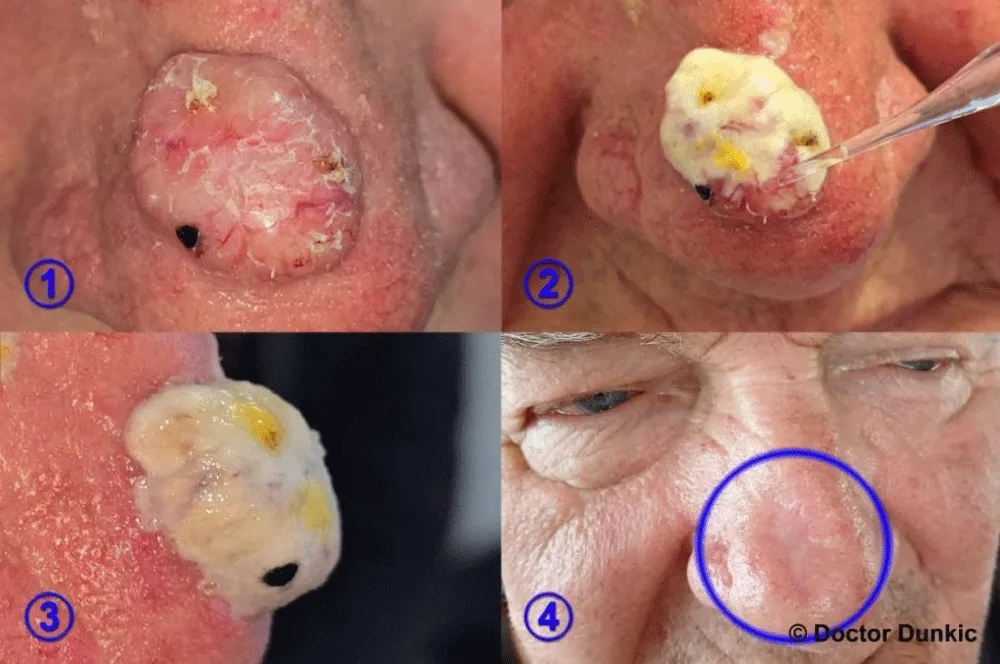
Figure 1 shows a dermoscopic view of nodular nonpigmented basal cell carcinoma in the patient described in this study. Transparent nodules with prominent arborizing blood vessels, characteristic of BCC, are clearly visible. Histopathological analysis was not possible because the tissue is instantly destroyed when applying the preparation according to the method of Dr. G. Dunkić. Consequently, no histopathological examination was performed, and the diagnosis, although supported by dermoscopic findings, remains presumptive and should be interpreted with caution.
Compared to cryotherapy or electrocautery, which may cause discomfort and require repeated sessions, the Dr. G. Dunkic method appears to offer a simpler and more patient-friendly procedure. Furthermore, the absence of immediate tissue destruction allows for gradual healing and epithelialization, which may be advantageous in cosmetically sensitive areas such as the nose (Figure 2).
The patient described here was not on immunosuppressive therapy; he has been receiving prescribed cardiological treatment for the past 15 years and reported no additional complaints (Figure 3).
The treatment was performed on 29.04.2024, and the final result (Figure 4) is from 21.08.2025. The treatment was sufficient to clear the lesion without the need for retreatment. The patient remained asymptomatic throughout the course, and the scab persisted for approximately 40 days before detaching spontaneously as a single piece.
The treatment involves the careful application of a liquid preparation to the surface of the lesion, during which the treated area turns white. As a result, the surrounding tissue becomes transiently bloody, but the redness resolves within approximately one hour. The procedure does not require anesthesia and is well tolerated, with the patient remaining comfortable and fully conscious throughout the procedure. The preparation does not spread to healthy tissue, and even if accidental contact occurs, the affected area recovers completely.
Conclusion
This case underscores the remarkable role of the patented chemical method developed by Dr. G. Dankić in the management of nodular, non-pigmented basal cell carcinoma of the nose. The intervention was straightforward, non-invasive, and resulted in the complete removal of the lesion with minimal scarring, thereby demonstrating its considerable value in anatomically sensitive regions where tissue preservation is of paramount importance. The application of Dr. Dankić’s method for lesion removal effectively circumvents the need for more complex procedures.
From a clinical standpoint, the favorable outcome in this patient suggests that such approaches may offer a simple and significantly more comfortable alternative for the removal of benign lesions, as well as those amenable to superficial excision but often associated with considerable discomfort. To date, a substantial number of lesions have been successfully treated using this technique, all with excellent results. Long-term follow-up has confirmed that even after 40 years of employing Dr. Dankić’s method, no complications have been observed, and patients have benefited not only in terms of aesthetic improvement but also in resolving health-related concerns straightforwardly.
Given the high incidence of skin cancer, particularly squamous cell carcinoma, in transplant recipients, it is important to highlight the potential application of Dr. G. Dunkić’s method in immunosuppressed patient populations. In one of our forthcoming manuscripts, we will present several case reports.
The participants were fully informed about the purpose, procedures, risks, and benefits of the study, which enabled them to make a voluntary and informed decision to participate. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Funding
No external funding was received for the preparation of this case report. The work was carried out independently within Health Care Clinic Apiderm Plus and Health Care Clinic Dunkic.
Acknowledgment
The authors would like to thank the Ministry of Science, Technological Development, and Innovation of the Republic of Serbia for the financial support of the research, the results of which are presented in the paper (contract 451-03-136/2025-03/200023).
References
- Djordjevic N, Dunkic A, Djordjevic M. Examples of removing benign lesions using the chemical method according to Dr. G. Dunkic. Glob J Med Clin Case Rep. 2025;159–60. Available from: https://doi.org/10.17352/2455-5282.000218
- Djordjevic N, Dunkic A. Chemical cosmetic method for removal of mole according to doctor Dunkic. 16th International Congress: Scientific Evidence in Unconventional Medicine, ExpoDiP digital platform. 2025. Available from: https://huped.hr/hr/clanci-detalji/camnet-baza-strucnih-tekstova-iz-nekonvencionalne-medicine/hemijska-kozmeticka-metoda-za-uklanjanje-mladeza-po-doktoru-dunkicu-61
- Sadek A, Oliveira A, Salerni G, Marín MB, Schwartz R, Cabo H. Nodular non-pigmented lesions on the face. In: Cabo H, Lallas A, editors. Atlas of Dermatoscopy Cases. Cham: Springer. 2020;43-52. Available from: https://doi.org/10.1007/978-3-030-43672-8_13
- Jacobi A, Mayer A, Augustin M. Keratolytics and emollients and their role in the therapy of psoriasis: a systematic review. Dermatol Ther (Heidelb). 2015;5(1):1–18. Available from: https://doi.org/10.1007/s13555-015-0068-3
- Sadick NS, Coutanceau C, Sibaud V, Merial-Kien C. Efficacy and safety of a new topical keratolytic treatment for localized hyperkeratosis in adults. J Drugs Dermatol. 2010;9(12):1512–1517. Available from: https://pubmed.ncbi.nlm.nih.gov/21120259/
- Steeb T, Koch EA, Wessely A, Wiest LG, Schmitz L, Berking C, et al. Chemical peelings for the treatment of actinic keratosis: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2021;35(3):641–9. Available from: https://doi.org/10.1111/jdv.16844
- Heppt MV, Steeb T, Leiter U, Berking C. Efficacy of photodynamic therapy combined with topical interventions for the treatment of actinic keratosis: a meta-analysis. J Eur Acad Dermatol Venereol. 2019;33(5):863–73. Available from: https://doi.org/10.1111/jdv.15459
- Heppt MV, Steeb T, Ruzicka T, Berking C. Cryosurgery combined with topical interventions for actinic keratosis: a systematic review and meta-analysis. Br J Dermatol. 2019;180(4):740–8. Available from: https://doi.org/10.1111/bjd.17435
- Pangti R, Gupta S. Surgical removal of moles. CosmoDerma. 2021;1(1):32. Available from: https://www.researchgate.net/publication/353332656_Surgical_removal_of_moles
- Ferrandiz L, Moreno-Ramírez D, Camacho FM. Shave excision of common acquired melanocytic nevi: cosmetic outcome, recurrences, and complications. Dermatol Surg. 2005;31(9):1112–1115. Available from: https://doi.org/10.1097/00042728-200509000-00005
- Tursen U, Kaya TI, Ikizoglu G. Round excision of small, benign, papular and dome-shaped melanocytic nevi on the face. Int J Dermatol. 2004;43(11):844–846. Available from: https://doi.org/10.1111/j.1365-4632.2004.02136.x
- Wang ECE, Sen P, Goh C, Chua S. Single treatment with 100-microsecond alexandrite laser clears selected acquired melanocytic nevi in type IV Asian facial skin. J Cutan Aesthet Surg. 2013;6(1):21–26. Available from: https://doi.org/10.4103/0974-2077.110092
- August PJ, Ferguson JE, Madan V. A study of the efficacy of carbon dioxide and pigment-specific lasers in the treatment of medium-sized congenital melanocytic naevi. Br J Dermatol. 2011;164(5):1037–42. Available from: https://doi.org/10.1111/j.1365-2133.2011.10236.x
- Scope A, Tabanelli M, Busam KJ, Rabinovitz H, Braun RP, Marghoob AA. Dispelling the myth of the “benign hair sign” for melanoma. J Am Acad Dermatol. 2007;56(3):413–6. Available from: https://doi.org/10.1016/j.jaad.2006.10.009
- Javate RM, Pamintuan FG. Endoscopic radiofrequency-assisted dacryocystorhinostomy with double stent: a personal experience. Orbit. 2005;24(1):15–20. Available from: https://doi.org/10.1080/01676830590890864
- Ragab SM. Bipolar radiofrequency dissection tonsillectomy: a prospective randomized trial. Otolaryngol Head Neck Surg. 2005;133(6):961–6. Available from: https://doi.org/10.1016/j.otohns.2005.07.037
- Scarano A, Carinci F, Candotto V, Lorusso F. Eradication of benign skin lesions of the face by voltaic arc dermabrasion (atmospheric plasma): postoperative pain assessment by thermal infrared imaging. Aesthet Plast Surg. 2020;44(8):2277–85. Available from: https://doi.org/10.1007/s00266-020-01891-z
- Ghadgepatil SS, Gupta S, Sharma YK. Clinicoepidemiological study of different types of warts. Dermatol Res Pract. 2016;2016:7989817. Available from: https://doi.org/10.1155/2016/7989817
- Bruggink SC, Eekhof JA, Egberts PF, van Blijswijk SC, Assendelft WJ, Gussekloo J. Natural course of cutaneous warts among primary schoolchildren: a prospective cohort study. Ann Fam Med. 2013;11(5):437–441. Available from: https://doi.org/10.1370/afm.1508




 Save to Mendeley
Save to Mendeley

