Global Journal of Medical and Clinical Case Reports
Asynchronous Bilateral Intravaginal Testicular Torsion in a 17-year-old Boy
1Medicana Medical Center, Sarajevo, Bosnia and Herzegovina
2Clinic for Pediatric Surgery, Clinical Center of the University of Sarajevo, Bosnia and Herzegovina
3Department of Radiology, Clinical Center of the University of Sarajevo, Bosnia and Herzegovina
4Clinic for Anesthesia and Resuscitation, Clinical Center of the University of Sarajevo, Bosnia and Herzegovina
5Clinical Pathology, Cytology and Human Genetics, Clinical Center of the University of Sarajevo, Bosnia and Herzegovina
6Clinic for Gynecology and Obstetrics, Clinical Center of the University of Sarajevo, Bosnia and Herzegovina
Author and article information
Cite this as
Badžak Dž, Karamustafić A, Jonuzi A, Karavdić K, Popović N, Kubat M, et al. Asynchronous Bilateral Intravaginal Testicular Torsion in a 17-year-old Boy. Glob J Medical Clin Case Rep. 2026:13(2):023-025. Available from: 10.17352/gjmccr.000240
Copyright License
© 2026 Badžak Dž, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Abstract
Asynchronous testicular torsion refers to testicular torsion occurring at different times on each side (i.e., torsion of one testis followed later by torsion of the contralateral testis), rather than both testes twisting simultaneously. A 17-year-old boy was referred to the Clinic twice as an emergency. The first time was due to torsion of the left testicle. After a physical examination and echo Doppler, the patient underwent urgent surgery, and a right testicle detorsion was performed, with the testicle being saved. We did not fix the left testicle. The second time, two months later, he came to our clinic because of torsion of the right testicle. We operated patient urgently without a preoperative Doppler. The second testicle was also operated on in time.
Introduction
Clinically, asynchronous bilateral testicular torsion most commonly involves intravaginal torsion, in which the testis rotates within the tunica vaginalis membrane [1]. A clinical prerequisite for this is the “bell-clapper deformity”, an abnormal anatomical attachment of the testis to the scrotum, allowing freer rotation. Testicular torsion typically presents with sudden, severe pain and swelling in one testicle, often accompanied by nausea and vomiting. The affected testis is usually elevated with an abnormal lie, and the cremasteric reflex is absent on the involved side [2].
Asynchronous testicular torsion refers to testicular torsion occurring at different times on each side (i.e., torsion of one testis followed later by torsion of the contralateral testis), rather than both testes twisting simultaneously [3]. Synchronous testicular torsion refers to the rare event when both testes twist (torsion) at the same time, causing acute bilateral testicular ischemia. It’s much less common than asynchronous (sequential) torsion [3]. Ultrasound with Color Doppler analysis is crucial for assessing blood flow in the testes and confirming the diagnosis [4]. Treatment is usually surgical, involving detorsion and fixation (orchidopexy) of both testes to prevent recurrent torsion [4].
Case report
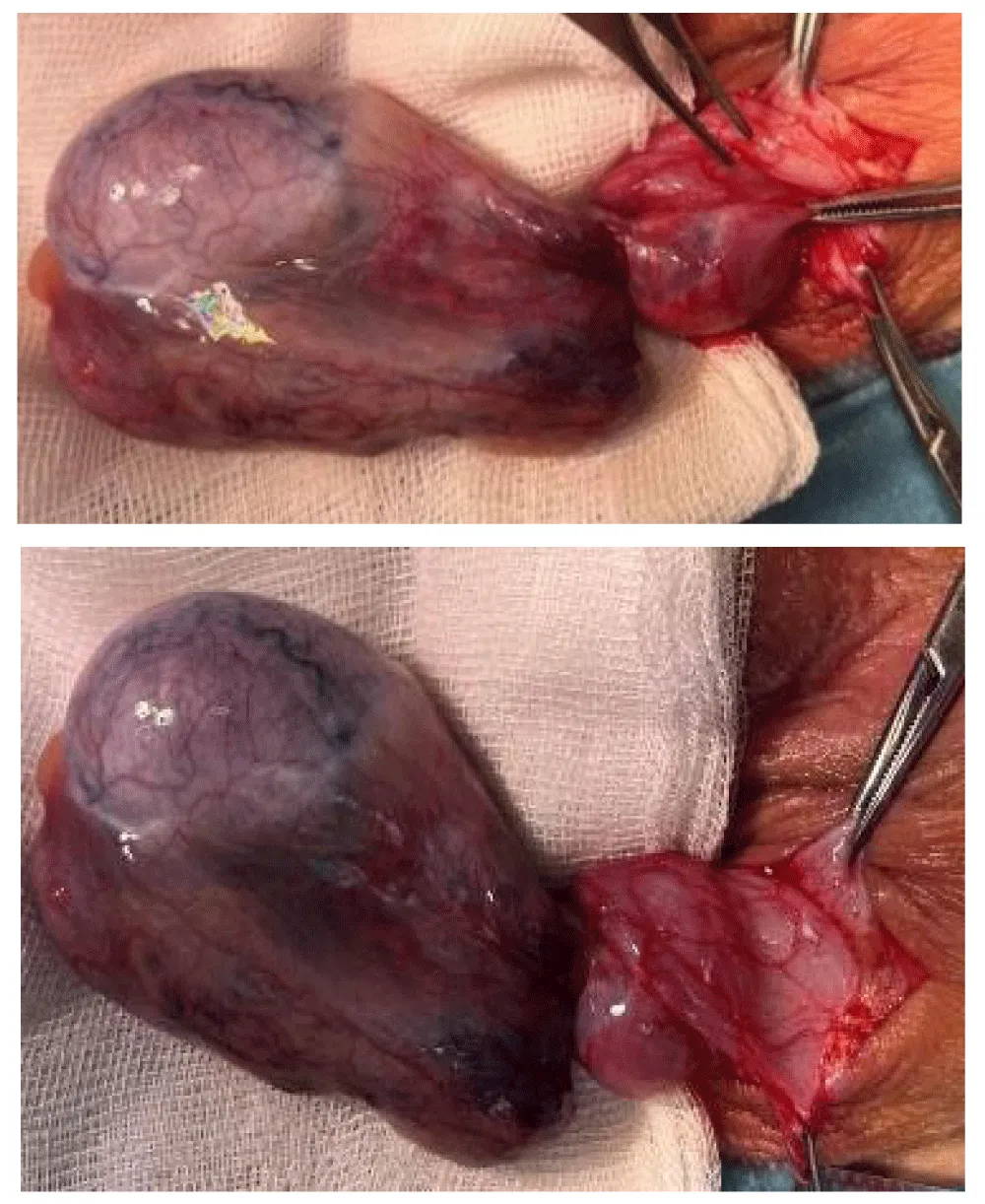
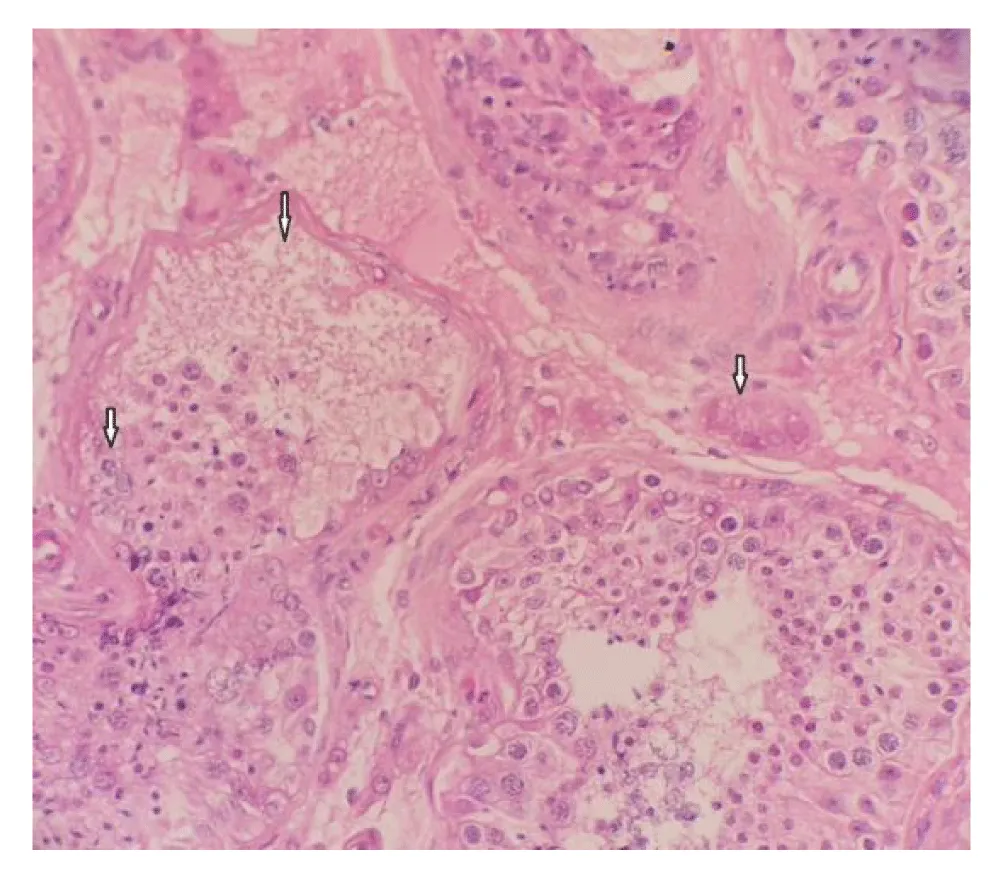
A 17-year-old boy was referred to the Clinic on February 11, 2025, due to pain and swelling of the left testicle. The swelling and pain have been present for the past 9 hours. He denies any trauma. Physical examination: The skin of both testes is normal in colour; the cremasteric reflex is absent. The left testis is palpably tender to palpation in the transverse position. An urgent testicular ultrasound with Color Doppler analysis and laboratory tests was performed. The ultrasound showed a whirlpool sign of the left spermatic cord, with an edematous epididymis. Color Doppler analysis revealed no detectable vascularization. A small hydrocele and edema of the soft tissues of the left hemiscrotum were also observed. Inflammatory markers and laboratory results are within normal limits. Surgical intervention is indicated based on suspicion of torsion of the left testis. Under general anesthesia, a transverse incision was made to access the testis, which was found to be softer in consistency and intravaginally twisted 540 degrees (Figure 1,2). Testicular viability was preserved; therefore, it was decided to retain and fixate the testis. A testicular biopsy was taken during the surgery. Testicular biopsy pathohistologically showed preserved seminiferous tubules with preserved spermatogenesis. Congestion of blood vessels and mild interstitial edema were present. Incipient necrosis of individual cells was seen in two canaliculi (Figure 3). Anticoagulant therapy was initiated, along with antibiotic treatment using a cephalosporin and analgesics. Locally, cold compresses were applied. The early postoperative course was uneventful. The first follow-up is scheduled for 7 days—both testicles are in the scrotum, and the surgical wound is healing well. The next follow-up is planned in one month, including testicular ultrasound with volumetry and Color Doppler analysis. We did not perform bilateral orchidopexy in the same procedure because it is standard at our Clinic. Contralateral orchidopexy is planned to be performed after 3 months due to inflammatory changes in the affected testicle and surrounding tissue.
Two and a half months after the first surgery, the boy was referred by a urologist from the hospital due to pain in the right testis. The swelling and pain have been present for the past hour. He denies any trauma. On physical examination, hyperemia of the right side of the scrotum is present. The cremasteric reflex is absent, and the right testis is palpably tender. Due to a high degree of suspicion, only laboratory tests were performed without a preoperative ultrasound with Doppler analysis. Under general anesthesia, a longitudinal incision is made along the scrotal skin. The tunica layers of the testis are opened, revealing the testis, which appears normal in color and is intravaginally torsed by 540 degrees (Figure 4). Testicular fixation is then performed. Postoperative follow-up and ultrasound showed normal blood flow and appearance of the testicle. We followed the patient for 3 months.
Discussion
Asynchronous bilateral testicular torsion is a rare but urgent surgical condition. In our case, the first testis was treated successfully, while the contralateral testis was not fixed due to normal vascularization and physical exam findings. This case reinforces the recommendation for bilateral orchidopexy in all patients presenting with testicular torsion to prevent asynchronous or bilateral torsion. A comprehensive surgical approach, including fixation of both testes, is essential to prevent recurrence and preserve testicular function.
Although there are not many reported cases in the literature related to asynchronous testicular torsion, from the available data, it can be concluded that in most cases involving newborns, exploration of the contralateral testis is performed regardless of the presence of clinical signs indicating torsion of the second testis.
As described in the article by Granger and Brownlee, where they reported right testicular torsion with discoloration of the right testis, the contralateral (left) testis was also explored, and bilateral torsion was confirmed [5].
The recommendation for exploration of the contralateral testis in the neonatal period is based, in addition to the possibility of synchronous torsion of the contralateral testis, on the fact that most extravaginal neonatal torsions end with orchidectomy. Therefore, it is recommended that the contralateral testis be explored and fixed in the same procedure to prevent possible future torsion [5].
According to the study by Elizabeth B. Yerkes and Frank M. Robertson, published in the article ‘Management of Perinatal Torsion: Today, Tomorrow or Never’ in the Official Journal of the American Urological Association, clinical examination in 18 patients suggested unilateral perinatal torsion. However, in 4 cases, contralateral torsion was discovered during surgical exploration. Despite orchiopexy of the better-perfused testis, all 4 cases resulted in testicular atrophy. No anesthesia- or surgery-related complications were reported [6].
According to an article published in Urology Research and Practice by Pakmanesch H. and Alinejad M., a case of bilateral torsion was presented with unilateral scrotal swelling, accompanied by atrophy and dark discoloration of the contralateral testis. This case report highlights that bilateral exploration is mandatory in every case of perinatal testicular torsion. This approach allows evaluation of the contralateral testis and fixation to prevent future torsion [7].
According to the study by E. Hynes, color Doppler ultrasound is not always a reliable indicator for ruling out testicular torsion. Among 16 patients with testicular torsion, the Doppler findings were falsely negative in 5 cases. The study concluded that the high number of false-negative results makes Doppler imaging unreliable for excluding the diagnosis of testicular torsion [8].
The literature describes various scenarios, including bilateral torsion that remained unrecognized due to a normal physical examination or normal color Doppler findings on the contralateral testis, leading to a failure to explore or fix it. Additionally, cases of asynchronous torsion have been reported, where torsion of the opposite testis occurred hours, days, or even months after the initial event, despite normal Doppler imaging at the time.
Conclusion
Fixation of both testes during testicular torsion is considered essential due to the potential risk of contralateral torsion.
There is no evidence to suggest that the risk of anesthesia is significant enough to justify avoiding contralateral exploration and fixation.
Although intravaginal synchronous and asynchronous torsion is extremely rare in teenagers, due to possible catastrophic consequences, it is recommended to explore and fix the contralateral testicle in the same act.
References
- Osumah TS, Jimbo M, Granberg CF, Gargollo PC. Frontiers in pediatric testicular torsion: An integrated review of prevailing trends and management outcomes. J Pediatr Urol. 2018;14(5):394-401. Available from: https://pubmed.ncbi.nlm.nih.gov/30087037/
- Taghavi K, Dumble C, Hutson JM, Mushtaq I, Mirjalili SA. The bell-clapper deformity of the testis: The definitive pathological anatomy. J Pediatr Surg. 2021;56(8):1405-1410. Available from: https://doi.org/10.1016/j.jpedsurg.2020.06.023
- Shukla AR, Snyder HM. Disorders of the testes and scrotum. In: Kavoussi LR, Partin AW, Peters CA, editors. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia: Elsevier; 2020.
- Alexander CE, Warren H, Light A, Agarwal R, Asif A, Chow BJ, et al. Ultrasound for the diagnosis of testicular torsion: A systematic review and meta-analysis of diagnostic accuracy. Eur Urol Focus. 2025;S2405-4569(25)00104-X. Available from: https://doi.org/10.1016/j.euf.2025.04.026
- Granger J, Brownlee EM, Cundy TP, Goh DW. Bilateral perinatal testicular torsion: Successful salvage supports emergency surgery. BMJ Case Rep. 2016;2016:bcr2016216020. Available from: https://doi.org/10.1136/bcr-2016-216020
- Yerkes EB, Robertson FM, Gitlin J, Kaefer M, Cain MP, Rink RC. Management of perinatal torsion: Today, tomorrow, or never? J Urol. 2005;174(4 Pt 2):1579-1582. Available from: https://doi.org/10.1097/01.ju.0000179542.05953.11
- Pakmanesh H, Alinejad M. A case of bilateral perinatal testicular torsion that presented with unilateral torsion; necessity of contralateral testis exploration. Turk J Urol. 2018;44(6):511-514. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6179741/
- Elliott SD, Hynes HE. Doppler ultrasound failure in testicular torsion. Br J Urol. 1984;56(6):647-649. PMID:6391304. Available from: https://pubmed.ncbi.nlm.nih.gov/6391304/


 Save to Mendeley
Save to Mendeley

